"In thinking back to all the inpatient units I've been associated with (six) and the patients who were admitted to them (thousands), the most important thing we did for many was to stop the irrational medications they were prescribed by psychiatrists." Psychiatrist Michael Alan Taylor, M.D., in his book Hippocrates Cried: The Decline of American Psychiatry (Oxford University Press 2013, p. 167)
"There is no evidence that any class of psychiatric drug acts by reversing or partially reversing an underlying physical process that is responsible for producing symptoms." Joanna Moncrieff, MBBS, MSc, MRCPsych, MD — Senior Lecturer in Mental Health Sciences, University College, London, "Psychiatric diagnosis as a political device", Social Theory & Health, Vol. 8, 4, pp. 370-882 (2010)
"For every class of psychiatric drugs, long-term studies (a few months or more) have continued to show no proof of effectiveness. ... all psychiatric drugs have serious long-term adverse effects and tend to produce chronic brain impairment (CBI)." Psychiatrist Peter R. Breggin, M.D., in his book Psychiatric Drug Withdrawal—A Guide for Prescribers, Therapists, Patients, and Their Families (Springer Publishing 2013), pp. 70 & 265
"I'm someone who has been gravely harmed by psych drugs and just trying to pick up the pieces of my life to carry on with it. ... I've been off psych drugs for 4 years now and still debilitated by them. ... I'm continually astounded at the downward pull of these pills on my life even now. Makes me think that I must somehow help others from psychiatry when I recover myself." E.R., female, age 35, in Michigan, in e-mail to me in 2015
"I've lost everything. ... Klonopin took it all." L. A., female, age 55, New York, in a telephone conversation with me in 2014 or 2015
"...how then can we distinguish psychopharmacology from quackery?" Stuart A. Kirk, D.S.W., Tomi Gomory, Ph.D., & David Cohen, Ph.D., in their book Mad Science—Psychiatric Coercion, Diagnosis, and Drugs (Transaction Publishers 2013), p. 275
Psychiatric drugs harm the brain, often permanently. Psychiatric drugs have no beneficial effects for those who take them (except, sometimes, a placebo effect, if taken in a dose low enough for their toxic effects to not be pronounced—or relief of withdrawal symptoms when attempting to reduce dosage or stop taking the drug). Psychiatric drugs and the physicians, physician assistants, nurse practitioners, and (in some states of the U.S.A.) psychologists who prescribe them, and judges who order their administration, are dangers to your health. Legislators and governors who enact laws authorizing "treatment over objection" with psychiatric drugs, and judges who approve involuntary psychiatric "medication" orders, and those who carry out the orders, are subjecting people to misery and to brain-damage that is often not reversible, and they are violating human rights. Because government licensing of health care practitioners exists to protect the public from harmful or unscientific treatment, the use of psychiatric drugs by licensed practitioners should be prohibited by law—except for patients who are already addicted to a psychiatric drug and need to be withdrawn slowly, or who must continue taking a drug for life to avoid intolerable withdrawal symptoms.
Most of what you need to know about psychiatric drugs or "medications" is found in a 457 page book published in 2008 by psychiatrist Peter R.
Breggin, M.D., Brain-Disabling Treatments in Psychiatry, Second Edition (Springer Publishing Company):
...except for the brain dysfunction and biochemical imbalances caused by psychiatric drugs, there are no known abnormalities in the brains of people who routinely seek help from psychiatrists ... For this edition of this book, the concept of brain-disabling treatment has been updated and expanded with...new information on the neurotoxicity and cytotoxicity of all antipsychotic drugs. ... All biopsychiatric treatments share a common mode of action: the disruption of normal brain function. ... all the major categories of psychiatric drugs—antidepressants, stimulants, tranquilizers (antianxiety drugs), mood stabilizers, and antipsychotics—are neurotoxic. They poison neurons, and sometimes destroy them. ... The currently available biopsychiatric treatments are not specific for any known disorder of the brain. One and all, they disrupt normal brain function, without correcting any brain abnormality. ... even if one or another psychiatric disorder someday turns out to have a biological basis, that in no way would justify inflicting psychiatric drugs on these patients, thereby compounding their underlying brain disorder with drug toxicity. ... Ironically, psychiatric drugs do not cure or ameliorate central nervous system disorders; they cause them. [pp. xxiii, xxvii, 2, 7, 8, 43]
IF YOU'RE GETTING AN EFFECT FROM A
PSYCHIATRIC DRUG, IT'S A DISABLING EFFECT.
_________________________________________________
As Dr. Breggin makes clear in Brain-Disabling Treatments in Psychiatry and several other books, and as journalist Robert Whitaker documents in Anatomy of an Epidemic (see Recommended Reading at the end of this essay), and as I will show in more detail in what follows, psychiatry has no medications. Psychiatry has drugs. While it isn't apparent from their medical dictionary definitions, as the words have come to be used, "drug" and "medication" are not entirely synonymous. The word "medication" implies benefit. The word "drug" does not necessarily. For example, heroin and cocaine are drugs, but I've never seen or heard anyone call either a medication. This is why advocates of psychiatric drugs usually call them "medication" and critics usually call the same substances "drugs". All medications are drugs, but a chemical or compound can be a drug without being a medication. All of psychiatry's drugs fall outside the usual meaning of the word medication because they do not help and in many if not most cases inflict harm. Another reason psychiatric drugs are not medications is medication, by the usual definition, cures or reduces the symptoms of a disease (a disease, or illness, being an abnormality of the body that impairs its function), and no psychiatric drug does that. As Dr. Peter Breggin says (in the last sentence of the above indented quote), in psychiatry, "medication" is something that gives you a disease.
The idea of a mentally ill person being "stabilized on medication" is a myth perpetrated by pharmaceutical companies seeking to maximize profits by selling more of their "medications", biologically oriented psychiatrists and psychologists who prescribe them, drug company financed advocacy groups such as the National Alliance on Mental Illness (NAMI), and script writers for television shows and motion pictures who in their fictional accounts portray mentally ill people as violent or irrational when they stop taking their "medication". The reality is today people called mentally ill are not "stabilized on meds" but disabled by drugs. Because of their sedating effects, psychiatric drugs can temporarily suppress violent, irritating, or vexing thinking or behavior, but they also cause temporary and permanent damage to the brain and eventual behavioral problems and increase risk of death in persons taking them. Being not only neurotoxic but cytotoxic (which means poisonous to living cells in general), psychiatric drugs often harm not only the brain but harm other parts of the body, too. In Your Drug May Be Your Problem—How and Why to Stop Taking Psychiatric Drugs (Perseus Books 1999, p. 81), psychiatrist Peter Breggin and clinical social work professor David Cohen say neuroleptic or "antipsychotic" drugs "subject almost every system in the body to impairment. Research, including a recent study, indicates that these drugs are toxic to cells in general."
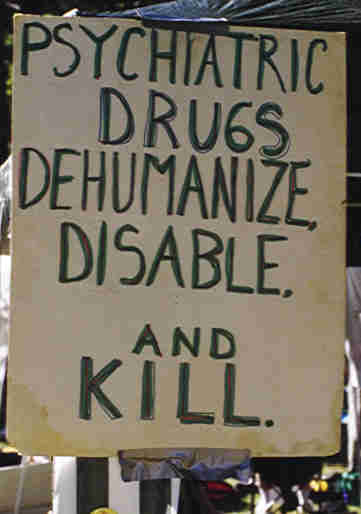
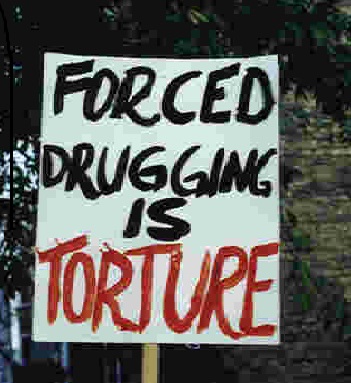
Testimony of psychiatrists and patients in involuntary civil commitment and treatment-over-objection hearings give the impression that about 90% of hospital psychiatry today consists of psychiatrists trying to force people to take their so-called medications and the "patients" trying to avoid them. Most psychiatric drugs make people feel miserable, so most people resist taking them. Psychiatric drugs are so harmful they should be taken by nobody, but they are forced upon patients in psychiatric hospitals. Many people living outside hospitals are court-ordered to take psychiatric drugs while living in their own homes or as a condition of release from a psychiatric hospital.
Punishing people by compelling them to take psychiatric drugs that make them feel bad and harm their health, while falsely believing or pretending the drugs are treating an illness, may force people to change their (outwardly expressed) ideas or their behavior to avoid this punishment, but this is not health care.
In his article, "A Critique of Psychiatry and an Invitation to Dialogue" (published in Ethical Human Science and Services, December 27, 2000), psychiatrist Ron Leifer, M.D., asks, "If mental illness is a social construct rather than a bodily illness, then questions naturally arise about the use psychiatric drugs. What does it mean to prescribe a drug for a metaphorical illness?" It means the use of psychiatric drugs is pseudoscience and quackery.
Because psychiatric drugs interfere with normal functioning of the brain (and hence the mind) and other parts of the human body and do not treat any bona-fide disease, their use is health care quackery, not health care.
PSYCHIATRY HAS HARMFUL DRUGS
BUT NO TRUE MEDICATIONS
_________________________________________________
In the 1970s when I sat in on a psychiatry class with a medical student friend, the professor told us "Research has shown we do not need to sleep, but we do need to dream." According to Jessica Payne, Ph.D., associate professor of psychology and director of the Sleep, Stress, and Memory Lab at the University of Notre Dame, "during sleep, your mind and body are actually highly active with processes critical for your physical and mental health. ... sleep is as important to your well-being as diet and exercise" (quoted in Real Simple magazine, realsimple.com, August 2014, p. 105 at 106). The dream phase of sleep, called the rapid eye movement (REM) phase, is the critical part. Contrary to the claim psychiatric drugs such as major and minor tranquilizers, so-called antidepressants, and mood stabilizers are useful as sleeping
pills, their real effect is to inhibit or block real sleep, particularly the critical REM or dream phase. In an article titled "The Effects of Antidepressants on Sleep", Andrew Winokur, M.D., Ph.D., Professor of Psychiatry and Director of Psychopharmacology at the University of Connecticut, and Nicholas DeMartinis, M.D., Assistant Clinical Professor at the University of Connecticut and an employee of Pfizer, Inc., say "Virtually all of the SSRIs [Selective Serotonin Reuptake Inhibitor antidepressants] have been noted to suppress REM sleep". They say "The majority of TCAs [Tri-Cyclic Antidepressants] markedly suppress REM sleep" and that the MAOIs (MonoAmine Oxidase Inhibitors) Phenelzine and Tranylcypromine used as antidepressants "have been demonstrated to produce REM suppression". They also say "with the selective SNRIs [Serotonin and Norepinephrine Reuptake Inhibitors, which is another class of supposedly antidepressant drugs], the general pattern of effects reported are ... disruption of sleep continuity and prominent suppression of REM sleep" (psychiatrictimes.com, June 13, 2012). In his lecture at the 2011
Empathic Therapy Conference in Syracuse, New York, psychiatrist and psychoanalyst Douglas C. Smith, M.D., of Juneau, Alaska said this:
Dreaming, it turns out, is absolutely essential to life. We cannot live without dreaming. There are experiments where you can deprive people of REM sleep, and they go crazy very quickly. If you do it with lab animals—'cause all mammals have REM sleep dreams—if you deprive lab animals of REM sleeping, they die sooner than they would of starvation. So we need to dream more than we need to eat. ... I worry about psychiatric medicines because—for many reasons, but here's another one, if you hadn't thought of this one—all psychoactive substances impair dreaming. They all inhibit or impair in some way the normal dreaming process, the REM cycle. You can see it with EEGs and the sleep studies. Even sleeping pills impair normal sleeping.
A self-help magazine advises: "Do not take sleeping pills unless under doctor's orders, and then for no more than 10 consecutive nights. Besides losing their effectiveness and becoming addictive, sleep-inducing medications reduce or prevent the dream-stage of sleep necessary for mental health" (Going Bonkers? magazine, premiere issue, p. 75). In his autobiography, Pulitzer Prize winning writer William Styron says after taking Nardil, Halcion, and Ativan, he did not dream for "many months" (Darkness Visible, Random House 1990, pp. 60, 70, 71, 75). Sleep deprivation experiments on normal people show loss of sleep causes hallucinations if continued long enough (according to Maya Pines in her book The Brain Changers, Harcourt Brace Jovanovich 1973, p. 105). So what would seem to be one of the likely consequences of taking drugs, such as psychiatric drugs, that inhibit or block real sleep? In psychiatry, where words and phrases imply or suggest the opposite of the truth, drugs that suppress the rapid eye movement or REM or dream phase of sleep, making a person more susceptible to hallucinations, are called "antipsychotic"! Many psychiatric drugs induce what looks like sleep to an uninformed or miseducated observer (which seems to include most mental health professionals), but the drugs actually induce a dreamless unconscious state—not sleep. By impairing REM sleep, psychiatric drugs cause rather than cure what is typically thought of as mental illness, which as Robert Whitaker documents in his book Anatomy of an Epidemic (Crown Publishers 2010), has become epidemic rather than being reduced or eliminated during psychiatry's psychopharmaceutical era starting in the 1950s and 1960s and continuing to the present day.
IN PSYCHIATRY, "MEDICATION" GIVES YOU A DISEASE
(RATHER THAN CURING or TREATING ONE)
_________________________________________________
Psychiatrist Douglas C. Smith also said this in the aforementioned lecture:
If you look at the research on lab animals that get deprived of REM sleep, they become kind of psychotic. They become aggressive. They can be violent. They actually become more, they call it, more instinctually driven. They want sex more, indiscriminately. They eat more. And they become more aggressive. Well, who does that remind you of? You know, of people that are on psychiatric drugs. I've heard stories today [at this conference] about some people that have become extremely violent—suicidal or aggressive [while taking psychiatric drugs]. ... One thing that's coming out in the psychiatric literature, there's more awareness now, especially with antidepressants—I think it might be all psychiatric drugs, psychoactive substances—but with antidepressants, there's data that with long-term use you have chronic insomnia. And boy, do I see that, more and more it seems like I'm seeing it [in my clinical practice].
The most dramatic examples of harm from psychiatric drugs are the deaths they cause, such as from neuroleptic malignant syndrome, neurological and cardiac problems caused by psychiatric drug toxicity, and people who become violent or suicidal when under the influence of a psychiatric drug who would not be if left in their normal unmedicated state. The effect of psychiatric drugs on the rapid eye movement phase of sleep is one explanation for psychiatric drug induced impulsivity, violence, suicide, and homicide. Another is something called frontal lobe syndrome.
In his book Borderline Personality Disorder in Adolescents (Fair Winds Press 2007, p. 82) Harvard psychiatry professor and medical director of the Adolescent Dialectical Behavioral Therapy Center at McLean Hospital Blaise A. Aguirre, M.D., says this about the frontal lobes of the brain:
The Frontal LobesThe frontal lobes are the part of the brain entrusted with executive function. This includes the ability to accomplish the following:
• Recognize future consequences resulting from current actions
• Choose between good and bad actions
• Hold and weigh opposing viewpoints
• Override and suppress unacceptable social responses
• Determine similarities and differences between things or events ...People who have had accidents or trauma that have damaged their frontal lobes often display irritability, impulsivity, and angry outbursts.
Do psychiatric drugs damage or disable the frontal lobes of the brain, causing people taking them to display "irritability, impulsivity, and angry outbursts" in the form of violence, homicide, and suicide? Psychiatrist Grace Jackson, M.D., suggests exactly this in her book Rethinking Psychiatric Drugs (AuthorHouse 2005, pp. 125-127, bold print in original):
A second possible mechanism of antidepressant-related suicide involves the impairment of activity within the frontal lobes. These brain regions are believed to be the critical centers of personality, impulse control, and executive functioning. Several teams of clinicians have been trailblazers in documenting the appearance of a reversible, amotivational syndrome in both adults and children treated with SSRIs [Selective Serotonin Reuptake Inhibitors, a category of supposedly antidepressant drugs]. Ultimately recognized by the prestigious Textbook of Psychiatry, the apathy syndrome refers to the delayed manifestation of behavioral changes in patients receiving serotonergic drugs, whose symptoms include apathy, flat affect, diminished motivation, and disinhibited actions. These features suggest a frontal lobe syndrome occurring eight weeks or more after the initiation of pharmacotherapy, or in many patients, after an increase in dose. One team of investigators corroborated the syndrome using neuroimaging studies in a 23-year-old patient who was treated with fluoxetine (Prozac) for obsessive compulsive disorder. In their research, the findings from SPECT [Single Photon Emission Computer Tomography] scans obtained before and after four months of daily medication revealed a 108% reduction in frontal lobe blood flow. These changes in blood flow paralleled reductions in motivation, attention, and memory, as well as decrements on neuropsychological tests designed to measure frontal lobe functions... Additional theories have been advanced as possible mechanisms of antidepressant-related violence. These include synergistic actions between alcohol and medication, whereby the disinhibiting effects of both substances hinder impulse control. Others have noted the potential for antidepressant therapy to provoke a wide variety of psychiatric symptoms, including mania, paranoia, hallucinations, panic attacks, or obsessive ruminations—all of which may contribute to suicidal and/or homicidal behaviors.
Psychiatrist Peter Breggin gives examples of people who became violent or suicidal in ways that were out-of-character for them in their unmedicated state in his book Medication Madness—The Role of Psychiatric Drugs in Cases of Violence, Suicide, and Crime (St. Martins Griffin 2009). Millions of people are prescribed psychiatric drugs that increase the risk they will become violent or suicidal, perhaps because of interference with the rapid eye movement or REM phase of sleep, perhaps by disabling the parts of the brain that would normally inhibit them from acting on angry or violent or suicidal impulses such as the frontal lobes. An eleven minute, twenty second YouTube video, "Psychiatric Drugs and Mass Shootings" includes many examples of psychiatric drugs seeming to cause homicide and suicide.
In her book The Predictor Scale: Predicting & Understanding Behaviors (Clifton Legacy Publishing 2013, p. 98), Faye Snyder, Psy.D., says "We have learned that some people react to anti-psychotics and anti-depressants in such a way that they become insanely psychotic, including acting out suicidal and homicidal fantasies."
Rather than correctly recognizing prescription psychiatric drugs as the problem, violence and suicide by people under the influence of psychiatric drugs have increased demands to "keep mentally ill people on their medication". Drug company advertising and biopsychiatric propaganda has been so successful, and fictional television crime shows and movies so misleading, that what in many cases caused the problem is thought of as the cure.
DRUG COMPANY ADVERTISING AND BIOPSYCHIATRIC PROPAGANDA HAS BEEN SO SUCCESSFUL, AND FICTIONAL TELEVISION CRIME SHOWS AND MOVIES SO MISLEADING, PSYCHIATRIC DRUGS THAT CAUSE VIOLENCE ARE THOUGHT
TO PREVENT VIOLENCE
_______________________________________________________
Today's perception of mental illness causing violence also confuses cause and effect in another way: People are not violent because they are mentally ill. They are called mentally ill because they are violent.
If psychiatric drugs are harmful, why do psychiatrists prescribe them?: First, they have been taught to do so. Second, they need to use medicine to establish and maintain their identity as medical doctors. As British psychiatrist Joanna Moncrieff says in her book The Bitterest Pills—The Troubling Story of Antipsychotic Drugs (Palgrave Macmillan 2013, p. 112), psychiatric drugs such as (so-called) antipsychotics are "central to the image that psychiatry was constructing of itself as a bona fide medial specialty." Third, using drugs insulates psychiatrists from competition from non-physician psychotherapists who cannot write prescriptions. Fourth, by writing a prescription, psychiatrists (and others with prescribing authority) can justify their fee even if they have no understanding of what is happening to a person psychologically or emotionally and can offer no helpful counselling.
Psychiatric drugs are good for psychiatrists and other prescribers. They are bad for patients.
Seeing the harm done by psychiatric "medication", Dr. Douglas Smith helps people slowly withdraw from them. At the 2011 Empathic Therapy Conference he also said—
One of the most pleasurable things about my work is seeing people come alive as they come off their [psychiatric] medicines. ... I mean, it's wonderful. ... To take a 28 year old young man that's been doped up, you know, on antipsychotics for a long time, and gradually work him off, and watch him come alive, it's so rewarding. It's one of the best things about what I do. ... It baffles me that psychologists are trying to get prescribing privileges.
You are probably wondering how psychiatric drugs get approval from government agencies such as the U.S.A.'s Food & Drug Administration (FDA) if they are as harmful as indicated here. There are several reasons.
One reason is former drug company executives who seem to have more loyalty to their former employers than to the public hold high positions within the FDA.
Another reason is FDA officials who have never worked for a drug company acquiesce to drug company proposals in hopes of gaining favor and being hired at eye-popping salaries by the companies they (theoretically) regulate during their stint at the FDA. In the words of Princeton University economics professor Paul Krugman in a book published in 2012—
Consider, for example, the revolving door, in which politicians and officials end up going to work for the industry they were supposed to oversee. That door has existed for a long time, but the salary you can get if the industry likes you is vastly higher than it used to be, which has to make the urge to accommodate the people on the other side of that door, to adopt positions that will make you an attractive hire in your postpolicy career, much stronger than it was thirty years ago. [End this Depression Now!, W.W.Norton & Co., p. 87]
In his book Pharmocracy (Praktikos Books 2011, p. 153), Life Extension Foundation Co-Founder William Faloon cites an Associated Press report saying "a record number of FDA employees are leaving the agency to go to work for pharmaceutical companies." He says "the FDA functions primarily to protect the financial interests of the pharmaceutical industry, not the public's health" (p. 152). In an article published in 2007, Marcia Angell, M.D., a senior lecturer at Harvard Medical School and former editor of the New England Journal of Medicine, says "The FDA now behaves as though the pharmaceutical industry is its user, not the public" ("Taking back the FDA", Boston Globe, February 26, 2007). Experts on FDA advisory panels are often simultaneously paid consultants for drug companies. According to Dr. Vernon Coleman, a British physician, "Governments say they can't find any doctors without conflict of interest to sit on committees assessing drugs" (Do Doctors And Nurses Kill More People Than Cancer?, European Medical Journal 2011, p. 34). Until this incestuous relationship between drug companies and the FDA is stopped by laws preventing anyone who has been employed by a drug company in recent years from serving at the FDA, and prohibiting FDA officials from accepting employment at drug companies for many years after leaving the FDA, and prohibiting experts on FDA advisory panels from accepting money from drug companies for many years before and after serving as consultants for the FDA, the FDA will probably continue to foster and protect the best interests of drug companies more than the best interests of the public.
Another reason for the approval of bad drugs is inadequate standards for drug approval. There must be two drug studies showing the drug being tested is better than a placebo (a pill with no active ingredients), with no limit on the number of studies that may be conducted in an effort to get the required two favorable studies. It doesn't matter if the drug company must do 100 studies to come up with 2 that show the proposed new drug is better than placebo. The other 98 studies showing the drug being tested is no better than or worse than a placebo will not prevent approval of the drug. As Peter R. Breggin, M.D. & David Cohen, Ph.D., say in their book Your Drug May Be Your Problem—How and Why to Stop Taking Psychiatric Medications (DaCapo/Perseus 2007, p. 7): "In order to approve a drug, the FDA requires only two positive studies, but drug companies invariably have to conduct many clinical trials before they can come up with a couple of positive clinical trials." Psychiatrist Daniel Carlat, M.D., in a lecture available on YouTube.com, says "The FDA's bar for proof of effectiveness is one of the lowest bars you can imagine" ("Daniel Carlat—Unhinged: The Trouble With Psychiatry", uploaded September 11, 2012, at 24:19).
Many critics also allege that allowing drug companies to control the studies needed for FDA approval of the company's drugs allows the drug company to manipulate the results. For example, in his book Overdosed America (Harper Perennial 2008, p. xvii), described on the front cover of the paperback edition as "How the pharmaceutical Companies Are Corrupting Science, Misleading Doctors, and Threatening Your Health", John Abramson, M.D., of the clinical faculty of Harvard Medical School says "Rigging medical studies, misrepresenting research results published in even the most influential medical journals, and withholding the findings of whole studies that don't come out in a sponsor's favor have all become the accepted norm in commercially sponsored medical research." In the first edition of Your Drug May Be Your Problem—How and Why to Stop Taking Psychiatric Drugs (Perseus Books 1999, pp. 189-190), Drs. Breggin and Cohen say—
But isn't psychiatry science? Isn't faith in psychiatry based on facts? On research? Can't we "trust in research"? The sad truth is that, in the field of psychiatry, it is impossible to "trust in research." Nearly all of the research in this field is paid for by drug companies and conducted by people who will "deliver" in the best way possible for those companies. ... Sadly, even well-informed people too often put their faith in psychiatry and psychiatric research. It is the same as putting their faith in a drug company.
In her book Side Effects—A Prosecutor, a Whistleblower, and a Bestselling Antidepressant on Trial (Algonquin Books 2008) Alison Bass shows how drug studies are deliberately falsified for the purpose of getting useless or harmful drugs approved and sold. She provides facts proving "that doctors who receive consulting or other personal income from drugmakers are more likely to report positive findings about a particular drug than researchers who don't receive money from the industry" and "psychiatry was the specialty with the highest number of doctors receiving payments from drug companies" (p. 224).
In his book Saving Normal—An Insider's Revolt Against Out-of-Control Psychiatric Diagnosis, DSM-5, Big Pharma, and the Medicalization of Ordinary Life (HarperCollins 2013, p. 212), psychiatrist Allen Frances says "The legal psychiatric drug industry has thrived through the aggressive spread of misinformation."
PEOPLE ARE NOT VIOLENT BECAUSE THEY ARE MENTALLY ILL. THEY ARE CALLED MENTALLY ILL BECAUSE THEY ARE VIOLENT.
__________________________________________________
Drug studies that are not paid for nor controlled by the drug company that is seeking approval for the drug are far more likely to show the drug is ineffective or harmful. The result is many drugs are approved for sale to the public that should not be. Government approval of a drug is little or no assurance of its effectiveness or safety. This is true for all drugs, not just psychiatric drugs.
Studies indicating psychiatric drugs are helpful are of dubious credibility not only because of dishonest drug company manipulation but also because of professional bias by psychiatrists employed in psychiatric drug testing. All or almost all psychiatric drugs are neurotoxic and for this reason cause symptoms and problems such as dry mouth, blurred vision, lightheadedness, dizziness, lethargy, difficulty thinking, menstrual irregularities, urinary retention, heart palpitations, and other consequences of neurological dysfunction. Psychiatrists deceptively call these "side-effects", even though they are the only real effects of today's psychiatric drugs. Placebos (or sugar pills) don't cause these problems. Since these symptoms (or their absence) are obvious to psychiatrists evaluating psychiatric drugs in supposedly double-blind drug trials, the drug trials aren't really double-blind, making it impossible to evaluate psychiatric drugs impartially. This allows professional bias to skew the results.
In the Introduction to his book The Great Psychiatry Scam—One Shrink's Personal Journey (Manitou Communications 2008, p. xii) psychiatrist Colin A. Ross, M.D., says "I will prove to you that over 90% of medication prescriptions for psychiatric inpatients have no scientific basis."
In her book The Myth of the Chemical Cure—A Critique of Psychiatric Drug Treatment, Revised Edition (Palgrave Macmillan 2009, p. 242) Joanna Moncrieff, M.B.B.S., M.Sc., MRCPsych, M.D., Senior Lecturer in the Department of Mental Health Sciences at University College London, U.K., says—
In retrospect the physical treatments of the mid-20th century, such as insulin coma therapy and frontal lobotomy, stand revealed as dangerous and degrading procedures perpetrated on vulnerable people in the name of medical progress. In the same way the multiple and long-term drugging of modern day psychiatric patients will surely some day be acknowledged as a dangerous fraud.
"ANTIDEPRESSANTS": The Comprehensive Textbook of Psychiatry/IV, published in 1985, says "The tricyclic‑type drugs are the most effective class of anti‑depressants" (Williams & Wilkins, p. 1520). But in his book Overcoming Depression, published in 1981, Dr. Andrew Stanway, a British physician, says "If anti-depressant drugs were really as effective as they are made out to be, surely hospital admission rates for depression would have fallen over the twenty years they've been available. Alas, this has not happened. ... Many trials have found that tricyclics are only marginally more effective than placebos, and some have even found that they are not as effective as dummy tablets" (Hamlyn Publishing Group, Ltd., p. 159-160). In his book Psychiatric Drugs—Hazards to the Brain, published in 1983, psychiatrist Peter Breggin, M.D., asserts "The most fundamental point to be made about the most frequently used major antidepressants is that they have no specifically antidepressant effect. Like the major tranquilizers [neuroleptics] to which they are so closely related, they are highly neurotoxic and brain disabling, and achieve their impact through the disruption of normal brain function. ... Only the 'clinical opinion' of drug advocates supports any antidepressant effect" of so-called antidepressant drugs (Springer Pub. Co., pp. 160 & 184). In another book published 30 years later, commenting not only on the older supposed antidepressants available in 1983 such as tricyclics (TCA's) and monoamine oxidase inhibitors (MAOI's), but also the newer so-called antidepressants such as selective serotonin reuptake inhibitors (SSRI's) like Prozac, and serotonin and norepinephrine reuptake inhibitors (SNRI's), and with the benefit of another 30 years of research to back-up his claim, Dr. Breggin says "It is now abundantly clear that antidepressants in the long-term make people more depressed and often disabled" (Psychiatric Drug Withdrawal, Springer Publishing 2013, p. 137). In her book The Myth of the Chemical Cure—A Critique of Psychiatric Drug Treatment (Palgrave MacMillan 2009), Joanna Moncrieff, M.B.B.S., M.Sc., MRCPsych, M.D., Senior Lecturer in the Department of Mental Health Sciences at University College London, U.K., includes three chapters on supposedly antidepressant "medications" (pp. 118-173) including a chapter titled "Is There Such a Thing as an 'Antidepressant'?" in which she concludes there is not. Psychologist Irving Kirsch, Ph.D., makes a similar argument in his book The Emperor's New Drugs—Exploding the Antidepressant Myth (Basic Books 2010).
Psychiatry professor Richard Abrams, M.D., has said "Tricyclic Antidepressants...are minor chemical modifications of chlorpromazine [Thorazine] and were introduced as potential neuroleptics" (in: B. Wolman, The Therapist's Handbook, p. 31). Being neuroleptics (marketed as antidepressants), they have the same harmful effects and risks. In his book Psychiatric Drugs—Hazards to the Brain, Dr. Breggin calls the tricyclic antidepressants "Major Tranquilizers in Disguise" (p. 166). Psychiatrist Mark S. Gold, M.D., has said antidepressants can cause tardive dyskinesia (The Good News About Depression, Bantam 1986, p. 259). (See below for my critique of neuroleptics.)
Evidence so-called antidepressants make people feel worse, not better, is found in a study of Paxil, a best selling so-called antidepressant in the selective serotonin reuptake inhibitor (SSRI) category: It was found that "'suicide-related events' occurred almost four times more often in patients taking Paxil than in those taking a sugar pill" (Alison Bass, Side Effects—A Prosecutor, a Whistleblower, and a Bestselling Antidepressant on Trial, Algonquin Books 2008, p. 221).
It is because of evidence of this sort that on October 15, 2004, the U.S. Food & Drug Administration (FDA) began "requiring black box warnings on all thirty-two antidepressants currently on the market, old [tricyclic, MOAI] as well as new [SSRI, SNRI]", advising doctors and patients that supposedly antidepressant drugs make people more rather than less likely to commit suicide (Id., p. 218). Such a warning wouldn't be needed if so-called antidepressants had the favorable effects their manufacturers and biologically oriented psychiatrists claim.
"WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
"Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term studies. These studies did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in patients over age 24..."
(FDA required warning in advertisements for supposedly antidepressant "medications")
__________________________________________________
The FDA warning (above) indicating so-called antidepressants do not promote suicidal thoughts and behavior in "patients over age 24" is obvious nonsense that probably reflects either poor design of the studies or bias by researchers: Why would a drug promote suicidal thoughts and behavior in a 21 year old but not a 31 year old?
In The Antidepressant Fact Book (Perseus 2001, p. 107) psychiatrist Peter R. Breggin, M.D., says "There are so many potential hazards involved in taking SSRIs that no physician is capable of remembering all of them and no patient can be adequately informed about the dangers without spending days or weeks reviewing the subject in a medical library."
LITHIUM, the classic "mood stabilizer" is said to be helpful for people whose mood repeatedly changes from joyful to despondent and back again. Psychiatrists call this manic-depressive disorder or bipolar mood disorder. Lithium was first described as a psychiatric drug in 1949 by an Australian psychiatrist, John Cade. According to a psychiatric textbook: "While conducting animal experiments, Cade had somewhat incidentally noted that lithium made the animals lethargic, thus prompting him to administer this drug to several agitated psychiatric patients." The textbook describes this as "a pivotal moment in the history of psychopharmacology" (Harold I. Kaplan, M.D. & Benjamin J. Sadock, M.D., Clinical Psychiatry, Williams & Wilkins 1988, p. 342). Apparently, the fact that lithium induces lethargy is the only rationale for its use. A supporter of lithium as psychiatric therapy admits lithium causes "a mildly depressed, generally lethargic feeling". He calls it "the standard lethargy" caused by lithium (Roger Williams, "A Hasty Decision? Coping in the Aftermath of a Manic-Depressive Episode", American Health magazine, October 1991, p. 20). One of my cousins was diagnosed as manic-depressive and was given a prescription for lithium carbonate. He told me, years later, "Lithium insulated me from the highs but not from the lows." It should be no surprise a lethargy-inducing drug like lithium would have this effect. Amazingly, psychiatrists sometimes claim lithium wards off feelings of depression even though lethargy-inducing drugs like lithium (like most psychiatric drugs) promote feelings of despondency and unhappiness—even if they are called antidepressants.
Lithium is often described by health care scientists and physicians as "toxic" and as capable of inflicting bodily harm. According to the National Kidney Foundation—
Lithium may cause problems with kidney health. ... The amount of kidney damage depends on how long you have been taking lithium. It is possible to reverse kidney damage caused by lithium early in treatment, but the damage may become permanent over time. [Lithium and Chronic Kidney Disease", kidney.org, accessed 7/21/2015]
Taking lithium makes people 30 times more likely to die (D. Ruschena, et al., "Choking deaths: the role of antipsychotic medication", British Journal of Psychiatry, Nov. 2003, Vol. 183, pp. 446-50, ncbi.nlm.nih.gov).
As with all biological treatment in psychiatry, lithium is administered as "treatment" for a "condition" or supposed mental illness for which there is no biological evidence.
MINOR TRANQUILIZERS (benzodiazepines): Included in this category are Ativan, Halcion, Klonopin, Librium, Valium and Xanax. Doctors who prescribe them say they have calming, anti-anxiety, panic-suppressing effects or are useful as sleeping pills. Anyone who believes these claims should read the article "High Anxiety" in the January 1993 Consumer Reports magazine, or read Chapter 11 in Toxic Psychiatry (St. Martin's Press 1991), by psychiatrist Peter Breggin, both of which allege the opposite is closer to the truth. British physician Vernon Coleman says "The benzodiazepines have caused infinitely more sorrow and despair than all illegal drugs put together" (benzo.org.uk, accessed January 15, 2015). Like all psychiatric drugs, the so-called minor tranquilizers don't cure anything but are merely brain-disabling drugs. In one clinical trial, 70 percent of persons taking Halcion "developed memory loss, depression and paranoia" ("Halcion manufacturer Upjohn Co. defends controversial sleeping drug", Miami Herald, December 17, 1991, p. 13A). According to the February 17, 1992 Newsweek, "Four countries have banned the drug outright" (p. 58). "Halcion has been categorically banned in the Netherlands" according to William Styron in his book Darkness Visible—A Memoir of Madness (Random House 1990, p. 71). Britain banned Halcion in 1991 ("Sleeping pill Halcion banned by Britain", Baltimore Sun, October 3, 1991, baltimoresun.com). Yet Halcion remains legal in the U.S.A.
In his book Saving Normal, psychiatrist and psychiatry professor Allen Frances, M.D., says this about Xanax and the FDA (HarperCollins 2013, p. 216):
Xanax has been more a wonder of profitability and longevity than a useful medication. Its therapeutic dosage is often high enough to be addicting, and its severe withdrawal anxiety is enough to keep patients hooked for life. Attempt at withdrawal may bring on severe panic or anxiety symptoms that are worse than the problems the patient started out with. Xanax is also a frequent collaborator with other prescription drugs and alcohol in iatrogenic overdoses and deaths. It has little role, if any, in the proper practice of medicine. If there was a proper war against prescription drug misuse, Xanax would be an early casualty—but under current policies the FDA has no mechanism to rein in drugs that do more harm than good.
In his book Toxic Psychiatry, psychiatrist Peter Breggin, speaking of the minor tranquilizers, says "As with most psychiatric drugs, the use of the medication eventually causes an increase of the very symptoms that the drug is supposed to ameliorate" (p. 246).
David Knott, a physician at the University of Tennessee, in 1976 warned: "I am very convinced that Valium, Librium and other drugs of that class cause damage to the brain. I have seen damage to the cerebral cortex that I believe is due to the use of these drugs, and I am beginning to wonder if the damage is permanent" (quoted in Robert Whitaker, Anatomy of an Epidemic, Crown Publishers 2010, p. 137).
ADHD DRUGS: Like all psychiatric "medications", drugs for attention deficit hyperactivity "disorder" (ADHD) are given for a supposed illness or condition nobody can show exists in a biological sense. Diagnosis is subjective. No laboratory test for ADHD exists. "There is no convincing evidence for either short- or long-term improvement in cognitive ability or academic performance" in those taking drugs for ADHD (Peter R. Breggin, M.D., Brain-Disabling Treatments in Psychiatry, Second Edition, Springer Publishing Co., 2008, p. 285). The harmful effects of drugs that supposedly treat ADHD include psychosis, mania, aggression, suicide, cardiovascular risks including heart attack, stroke, sudden death, brain atrophy, destruction of brain cells, permanent suppression of height and temporary suppression of weight (Id., pp. 296, 299, 307, 311, 315).
NEUROLEPTICS: Even as harmful as psychiatry's (so-called) antidepressants and lithium and (so-called) antianxiety agents (or minor tranquilizers) and ADHD drugs are, they are nowhere near as damaging as the neuroleptics, now most often (although incorrectly) called "antipsychotic" drugs. "Neuroleptic" means nerve-seizing. At one time these drugs were called "major tranquilizers", but over time the myth that they are anti-psychosis developed. Included in this category are "older" or "typical" neuroleptics such as Thorazine (chlorpromazine), Mellaril, Prolixin (fluphenazine), Compazine, Stelazine, and Haldol (haloperidol) and "newer" or "atypical" or "second generation" neuroleptics such as Abilify, Clozaril, Geodon, Invega, Latuda, Risperdal, Seroquel, and Zyprexa. Contrary to the often-repeated claim the newer or so-called atypical or second-generation neuroleptics are less likely than "older" or "typical" neuroleptics to cause neurological damage manifested by movement disorders, sometimes called "extrapyramidal side effects", such as tardive dyskinesia, dystonia, and akathisia, the National Institute of Mental Health (NIMH) Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study in 2005 found that "Contrary to expectations, movement side effects (rigidity, stiff movements, tremor, and muscle restlessness [dyskinesia, dystonia, and akathisia]) primarily associated with the older medications were not seen more frequently with perphenazine than with the newer drugs", perphenazine being one of the older or "typical" neuroleptics chosen because "perphenazine is an effective older antipsychotic that is less likely to produce EPS [extrapyramidal side effects]" than most "typical" or first-generation neuroleptics. This study found that "taken as a whole, the newer medications ["atypical" neuroleptics] have no substantial advantage over the older medication [perphenazine, the "typical" neuroleptic] used in this study" ("Questions and Answers About the NIMH Clinical Antipsychotic Trials of Intervention Effectiveness Study (CATIE) — Phase 1 Results", September 2005, available at www.nimh.nih.gov).
In terms of their psychological effects, these so-called antipsychotics, or major tranquilizers, cause misery—not tranquility. They reduce a person's ability to think and act. By disabling people, they can stop almost any thinking or behavior the "therapist" wants to stop. But this is simply disabling people, not therapy. The drug temporarily disables or permanently destroys good aspects of a person's personality as much as bad. In the words of Dr. Joanna Moncrieff, a British psychiatrist and Senior Lecturer in Mental Health Sciences at the University College, London, the neuroleptic or supposedly antipsychotic drugs are "not selective. They're not simply suppressing the psychosis. They're suppressing everything" ("Joanna Moncrieff—The Myth of the Chemical Cure—the Politics of Psychiatric Drug Treatment", February 25, 2013, YouTube.com, at 28:35).
Whether and to what extent the disability imposed by the drug can be removed by discontinuing the drug depends on how long the drug is given and at how great a dose. The neuroleptic, so-called major tranquilizer/"antipsychotic" drugs damage the brain more clearly, severely, and permanently than any others used in psychiatry. In his book Mad in America: Bad Science, Bad Medicine, and the Enduring Mistreatment of the Mentally Ill (Perseus 2002, p. 191) journalist Robert Whitaker says "Neuroleptics have been found to cause a dizzying array of pathological changes in the brain." Joyce G. Small, M.D., and Iver F. Small, M.D., both Professors of Psychiatry at Indiana University, criticize psychiatrists who use "psychoactive medications that are known to have neurotoxic effects", and speak of "the increasing recognition of long-lasting and sometimes irreversible impairments in brain function induced by neuroleptic drugs. In this instance the evidence of brain damage is not subtle, but is grossly obvious even to the casual observer!" (Behavioral and Brain Sciences, March 1984, Vol. 7, p. 34). According to Conrad M. Swartz, Ph.D., M.D., Professor of Psychiatry at Chicago Medical School, "While neuroleptics relieve psychotic anxiety, their tranquilization blunts fine details of personality, including initiative, emotional reactivity, enthusiasm, sexiness, alertness, and insight. ... This is in addition to side effects, usually involuntary movements which can be permanent and are hence evidence of brain damage" (Behavioral and Brain Sciences, March 1984, Vol. 7, pp. 37-38).
A report in the Mental and Physical Disability Law Reporter indicates some courts in the United States have considered involuntary administration of neuroleptic (so-called major tranquilizer or antipsychotic) drugs to involve First Amendment rights "Because ... antipsychotic drugs have the capacity to severely and even permanently affect an individuals' ability to think and communicate" ("Involuntary medication claims go forward", January-February 1985, p. 26, emphasis added).
In a concurring opinion in Rennie v. Klein, 720 F.2d 266 (3rd Cir 1983), three U.S. Court of Appeals judges (Weiss, et al.) said this:
Unlike the temporary and predictable effects of bodily restraints, the permanent side effects of antipsychotic drugs induce conditions that cannot be corrected simply by cessation of the regimen. The permanency of these effects is analogous to that resulting from such radical surgical procedures as a pre-frontal lobotomy.
For this reason, neuroleptic or "antipsychotic" drug use, especially when administered for a long time, has been called a "chemical lobotomy."
In Molecules of the Mind: The Brave New Science of Molecular Psychology, University of Maryland journalism professor Jon Franklin says "This era coincided with an increasing awareness that the neuroleptics not only did not cure schizophrenia—they actually caused damage to the brain." (Dell Pub. Co. 1987, p. 103). Psychiatry professor Richard Abrams, M.D., has acknowledged, "Tardive dyskinesia has now been reported to occur after only brief courses of neuroleptic drug therapy" (in: Benjamin B. Wolman (editor), The Therapist's Handbook: Treatment Methods of Mental Disorders, Van Nostrand Reinhold Co. 1976, p. 25). In his book The New Psychiatry, published in 1985, Columbia University psychiatry professor Jerrold S. Maxmen, M.D., says "The best way to avoid tardive dyskinesia is to avoid antipsychotic drugs altogether. Except for treating schizophrenia, they should never be used for more than two or three consecutive months. What's criminal is that all too many patients receive antipsychotics who shouldn't" (Mentor, pp. 155-156). In my opinion, Dr. Maxmen doesn't go far enough: His characterization of administration of neuroleptic (so-called antipsychotic or ma#or tranquilizer drugs) as "criminal" is accurate for all people, including those called schizophrenic, even when the drugs aren't given long enough for the resulting brain damage to show up as tardive dyskinesia.
In Psychiatric Drugs—Hazards to the Brain (Springer Pub. Co. 1983, pp. 70, 107, 135, 146) psychiatrist Peter Breggin, M.D., says this:
The major tranquilizers [neuroleptics] are highly toxic drugs; they are poisonous to various organs of the body. They are especially potent neurotoxins, and frequently produce permanent damage to the brain. ...tardive dyskinesia can develop in low-dose, short-term usage... the dementia [loss of higher mental functions] associated with the tardive dyskinesia is not usually reversible. ... Seldom have I felt more saddened or more dismayed than by psychiatry's neglect of the evidence that it is causing irreversible lobotomy effects, psychosis, and dementia in millions of patients as a result of treatment with the major tranquilizers.
POWER TO DRUG A PERSON BY FORCE
IS POWER TO DISABLE OR KILL HIM
________________________________________________________
In the same book Dr. Breggin, says that by using drugs that cause brain damage, "Psychiatry has unleashed an epidemic of neurological disease on the world" one which "reaches 1 million to 2 million persons a year" (pp. 109 & 108). In Brain-Disabling Treatments in Psychiatry, Second Edition (Springer Pub. Co. 2008, p. 62), Dr. Breggin says "The best approach to neuroleptics, in this author's opinion, is never to use them."
In Brain Disabling Treatments in Psychiatry, Second Edition (Springer Publishing Co. 2008, p. 112) Dr. Breggin says "prescribing physicians cannot fully inform patients about the risks associated with neuroleptics because no one except the most self-destructive patient would knowingly take such toxic drugs."
Critics of psychiatry say reform will not come from within psychiatry but must come from outside psychiatry, such as from the public, legislation, or judicial decisions. The author of the Preface of a book by four physicians (William E. Fann, M.D., et al., Tardive Dyskinesia: Research & Treatment, SP Medical & Scientific 1980) implicitly supports this view:
In the late 1960s I summarized the literature on tardive dyskinesia ... The majority of psychiatrists either ignored the existence of the problem or made futile efforts to prove that these motor abnormalities were clinically insignificant or unrelated to drug therapy. In the meantime the number of patients affected by tardive dyskinesia increased and the symptoms became worse in those already afflicted by this condition. ... there are few investigators or clinicians who still have doubts about the iatrogenic [physician caused] nature of tardive dyskinesia. ... It is evident that the more one learns about the toxic effects of neuroleptics on the central nervous system, the more one sees an urgent need to modify our current practices of drug use. It is unfortunate that many practitioners continue to prescribe psychotropics in excessive amounts, and that a considerable number of mental institutions have not yet developed a policy regarding the management and prevention of tardive dyskinesia. If this book, which reflects the opinions of the experts in this field, can make a dent in the complacency of many psychiatrists, it will be no small accomplishment." [Preface to: William E. Fann, M.D., et al., Tardive Dyskinesia: Research & Treatment, SP Medical & Scientific 1980]
These harmful so-called antipsychotic drugs are forced upon patients and prisoners despite being ineffective for their supposed purpose. In the second edition of their book Your Drug May Be Your Problem—How and Why to Stop Taking Psychiatric Medications (DaCapo/Perseus 2007, p. 101), Drs. Breggin and Cohen say "Contrary to claims, neuroleptics have no specific effects on irrational ideas (delusions) or perceptions (hallucinations)." Similarly, in his book Saving Normal—An Insider's Revolt Against Out-of-Control Psychiatric Diagnosis, DSM-5, Big Pharma, and the Medicalization of Ordinary Life, (Harper Collins 2013, p. 198, 199), psychiatrist Allen Frances, M.D., says people thought psychotic are given "atypical antipsychotic medications that have no proven efficacy. And most damning, these drugs have extremely dangerous complications." On the next page he says, "there is no proof whatever that antipsychotic medications are effective in preventing psychotic episodes."
Why, therefore, are these drugs called "anti-psychotic"?
In some studies, so-called antipsychotic or neuroleptic drugs have been found to cause rather than suppress psychosis. For example, in the U.S. Food & Drug Administrations (FDA's) "Focused Safety Review of Invega, March 14, 2013"—Invega being a so-called "atypical" supposedly anti-psychotic "medication"—it was found that "the most common serious AE [Adverse Event]" of taking Invega "was schizophrenia" ("Pharmaceutical Companies, the Largest Legal Settlements in US History and Illegal Marketing of Antipsychotic Drugs", by Attorney Stephen Sheller, at Dr. Peter Breggin's 2013 Empathic Therapy Conference, Syracuse, New York). Schizophrenia is generally considered a type of psychosis.
Calling drugs that cause psychosis "anti-psychotic" is typical of the misleading use of words in psychiatry. Psychiatry is a field in which words invert the truth: Drugs that make people more depressed are called "antidepressant". Drugs that make people more anxious, particularly during withdrawal, are called "anti-anxiety" or "anxiolytic". Toxic substances that cause disease are called "medication".
An article in a 2007 issue of Neuropsychopharmacology by scientists in the departments of psychiatry, statistics, and neuroscience at the University of Pittsburgh (Pennsylvania) said "Both in vivo [during life] and post-mortem investigations have demonstrated smaller volumes of the whole brain and of certain brain regions in individuals with schizophrenia. It is unclear to what degree such smaller volumes are due to the illness or to the effects of antipsychotic treatment." So researchers studied the effect of supposedly antipsychotic or neuroleptic drugs on monkeys, since only humans, not monkeys, are thought to be capable of having schizophrenia. They found "chronic exposure of macaque monkeys to haloperidol [Haldol, a "typical" antipsychotic] or olanzapine [Zyprexa, an "atypical" antipsychotic], at doses producing [blood] plasma levels in the therapeutic range in schizophrenia subjects, was associated with significantly smaller total brain weight and volume, including an 11.8-15.2% smaller gray matter volume in the left parietal lobe." The study suggests reduced brain size in individuals who take neuroleptic/antipsychotic "medications" are due to "antipsychotic"/neuroleptic "medications", not "schizophrenia" (Glenn T. Konopaske, et al., "Effect of Chronic Exposure to Antipsychotic Medication on Cell Numbers in the Parietal Cortex of Macaque Monkeys", Neuropsychopharmacology, Vol. 32, pp. 1216-1223).
The brain-damaging effect of supposedly antipsychotic drugs was also confirmed in an article in the February 2011 Archives of General Psychiatry that reported on a study of "Two hundred eleven patients with schizophrenia who underwent repeated neuroimaging". The study found "smaller brain tissue volumes and larger cerebrospinal fluid volumes. Greater intensity of antipsychotic [neuroleptic] treatment was associated with indicators of generalized and specific brain tissue reduction... More antipsychotic treatment was associated with smaller gray matter volumes. Progressive decrement in white matter volume was most evident among patients who received more antipsychotic treatment" (Beng-Choon Ho, MRCPsych; Nancy C. Andreasen, M.D., Ph.D., Steven Ziebell, B.S., Ronald Pierson, M.S., Vincent Magnotta, Ph.D., "Long-term Antipsychotic Treatment and Brain Volumes: A Longitudinal Study of First-Episode Schizophrenia", Vol. 68, No. 2, pp. 128-137).
The most severe side-effect of neuroleptics is death from neuroleptic malignant syndrome and other neurological malfunction caused by these "medications" such as cardiac arrhythmia (uncoordinated heartbeat). In Brain-Disabling Treatments in Psychiatry, Second Edition (Springer Publishing Co. 2008, p. 83), Dr. Breggin cites Gill, et al., in 2007 finding "Both the older and the atypical neuroleptics were associated with in increased risk of death at all assessment times, including 180 days, by a factor of 1.31-1.55 times."
Why do the so-called patients accept such "medication"? Sometimes they do so because of ignorance about the neurological damage and risk of death to which they are subjecting themselves by following their physician's or psychiatrist's advice to take the "medication". But much if not most of the time, neuroleptic drugs are literally forced into the bodies of the "patients" against their will. In his book Psychiatric Drugs—Hazards to the Brain, psychiatrist Peter Breggin, M.D., says "Time and again in my clinical experience I have witnessed patients driven to extreme anguish and outrage by having major tranquilizers forced on them. ... The problem is so great in routine hospital practice that a large percentage of patients have to be threatened with forced intramuscular injection before they will take the drugs" (p. 45).
Not only is this a kind of tyranny, but the forced administration of a psychiatric drug can be compared, physically and morally, with rape. Compare sexual rape and involuntarily administration of a psychiatric drug injected intramuscularly into the buttocks, which is a part of the anatomy where the injection is often given: In both sexual rape and involuntary administration of a psychiatric drug, force is used. In both cases, the victim's pants are pulled down. In both cases, a tube is inserted into the victim's body against her (or his) will. In the case of sexual rape, the tube is a penis. In the case of what could be called psychiatric rape, the tube is a hypodermic needle. In both cases, a fluid is injected into the victim's body against her or his will. In both cases it is or may be in (or near) the derriere. In the case of sexual rape the fluid is semen. In the case of psychiatric rape, the fluid is Thorazine, Prolixin or some other brain-disabling drug. The fact of bodily invasion is similar in both cases if not (for reasons I'll explain) actually worse in the case of psychiatric rape. So is the sense of outrage in the mind of the victim of each type of assault. (Victims of electroshock or ECT which was forced on them typically feel the same way.) Some who are not "hospitalized" (that is, imprisoned) are required to report to a doctor's office for injections of a long-acting neuroleptic like Prolixin every two weeks by the threat of imprisonment ("hospitalization") and forcible injection of the drug if they don't comply.
Why is psychiatric rape worse than sexual rape? As brain surgeon I. S. Cooper, M.D., says in his autobiography: "It is your brain that
sees, feels, thinks, commands, responds. You are your brain. It is you. Transplanted into another carrier, another body, your brain would supply it with your memories, your thoughts, your emotions. It would still be you. The new body would be your container. It would carry you around. Your brain is you" (The Vital Probe: My Life as a Brain Surgeon, W.W.Norton & Co. 1982, p. 50, emphasis in original). The most essential and most intimate part of you is not what is between your legs but what is between your ears. An assault on a person's brain such as involuntary administration of a brain-disabling or brain-damaging "treatment" (such as a psychoactive drug or electroshock or psychosurgery) is a more intimate and morally speaking more horrible crime than sexual rape. Psychiatric rape is in moral terms a worse crime than sexual rape for another reason, also: The involuntary administration of psychiatry's biological "therapies" cause permanent impairment of brain function. In contrast, women usually are still fully sexually functional after being sexually raped. They suffer psychological harm, but so do the victims of psychiatric assault. I hope I will not be understood as belittling the trauma or wrongness of sexual rape if I point out that I have counselled sexually raped women in my law practice and that each of the half-dozen or so women I have known who have been sexually raped have gone on to have apparently normal sexual relationships, and in most cases marriages and families. In contrast, the brains of people subjected to psychiatric assault often are not as fully functional because of the physical, biological harm done by the "treatment".
AN ASSAULT ON A PERSON'S BRAIN, SUCH AS
INVOLUNTARY ADMINISTRATION OF A PSYCHIATRIC DRUG,
IS A MORE INTIMATE ASSAULT THAN SEXUAL RAPE
_________________________________________________
In his interview with Dr. Joanna Moncrieff on 10/23/2013, psychiatrist Peter Breggin said this about the so-called antipsychotic, or neuroleptic "medications":
I feel more strongly, that we do know where we stand, that they are toxins. They ruin brain function, ultimately. They're shortening lifespans, in some studies indicating up to twenty years being lopped off peoples' lives on these drugs long term. I feel more strongly that in fact they're just a disaster, that we'd do better without them, and that in a sane society they'd be illegal. ... The [psychiatric] profession just refuses to look at this because...it threatens it's very core, its very identity. It's like taking a hammer away from a carpenter, maybe even the nails, too. [Dr. Peter Breggin Hour at 42:30, underline added]
Similarly, a year later in 2014 British psychiatrist Joanna Moncrieff said "I've found that the psychiatric establishment really does not want to engage in discussion of this issue of what its drugs are actually doing, possibly because that is just too dangerous and too difficult to rebut" ("Madness, Drugs and Capitalism: an Exploration by Dr. Joanna Moncrieff" YouTube.com, November 18, 2014, at 39:45).
A report by the National Association of State Mental Health Program Directors, "Morbidity and Mortality in People with Serious Mental Illness", in October 2006, states in bold italics, "People with serious mental illness (SMI) die, on average, 25 years earlier than the general population. State studies document recent increases in death rates over those previously reported" (p. 5). These increased death rates correspond with the advent and increase in use of psychiatric drugs. In Brain-Disabling Treatments in Psychiatry, Second Edition, psychiatrist Peter Breggin says "Until the advent of neuroleptic drugs, it was observed that patients diagnosed with schizophrenia lived normal life spans" (p. 82). Now that people thought to have serious mental illness such as "schizophrenia" are being drugged, they are dying 25 years sooner than average.
Psychiatrists continue damaging and killing "patients" with "medications" rather than admit psychiatric drugs are harmful—and lethal if taken long enough—because it is difficult for them to acknowledge the harm they have inflicted and continue to inflict on their patients, and because widespread recognition of what psychiatric drugs really do would bring about the end of psychiatry as a profession.
Since psychiatric drugs are not effective and have horrible, even lethal, effects on health, why are legislatures and courts authorizing their involuntary administration? The answer is legislators and judges sincerely believe mental illness (a) exists, and (b) is caused by biological abnormalities that can corrected by drugs. They are, in other words, misinformed. Instead of authorizing involuntary administration of psychiatric drugs, lawmakers and judges should be prohibiting their use (with the exception of attempts at phased withdrawal for people who are already taking them).
On a TV talk show in 1990, psychoanalyst Jeffrey Masson, Ph.D., said he hopes those responsible for harmful psychiatric "therapies" will one day face "Nürnburg trials" (Geraldo, Nov. 30, 1990).
These very same brain-damaging (so-called) neuroleptic/antipsychotic drugs are routinely administered—involuntarily—to mentally healthy old people in nursing homes in the United States. According to an article in the September/October 1991 issue of In-Health magazine, "In nursing homes, antipsychotics are used on anywhere from 21 to 44 percent of the institutionalized elderly... half of the antipsychotics prescribed for nursing home residents could not be explained by the diagnosis in the patient's chart. Researchers suspect the drugs are commonly used by such institutions as chemical straightjackets—a means of pacifying unruly patients" (p. 28). I know of two examples of feeble old men in nursing homes who were barely able to get out of their wheelchairs who were given a neuroleptic/antipsychotic drug. One complained because he was strapped into a wheelchair to prevent his attempts to walk with his cane. The other was strapped into his bed at night to prevent him from getting up and falling when going to the bathroom, necessitating defecating in his bed. Both were so physically disabled they posed no danger to anyone. But both dared complain bitterly about how they were mistreated. In both cases the nursing home staffs responded to these complaints with injections of Haldol—mentally disabling these men, thereby making it impossible for them to complain.
Despite various unverified theories and claims, psychiatrists don't know how the drugs they use work biologically. In the words of Columbia University psychiatry professor Jerrold S. Maxmen, M.D.: "How psychotropic drugs work is not clear" (The New Psychiatry, Mentor 1985, p. 143). According to the Psychopharmacology Institute web site (psychopharmacologyinstitute.com ©2015, accessed Feb. 20, 2015), edited by Flavio Guzman, M.D., a psychiatrist and Adjunct Professor of Pharmacology and Neurosciences at the University of Mendoza, "The exact mechanism of action of antipsychotic drugs is unknown."
All of today's commonly used psychiatric drugs suppress brain and other nervous system function, even basic functions such as heartbeat and motor control. The result is deaths from cardiac irregularities in persons taking supposedly antipsychotic drugs, and iatrogenic (physician-caused) neurological diseases such as tardive dyskinesia, dystonia, akathisia, and drug-induced dementia.
None of today's psychiatric drugs have the specificity (e.g., for depression or anxiety or psychosis) that is often claimed for them. In The Truth About the Drug Companies (Random House 2005, p. 82), Marcia Angell, M.D., says "In 1987, the FDA approved Prozac for the treatment of depression; in 1994, for the treatment of obsessive-compulsive disorder; in 1996, for bulimia". In his book Blaming the Brain—The Truth About Drugs and Mental Health (Free Press 1998, p. 105), Elliot Valenstein, Ph.D., Professor Emeritus of Psychology and Neuroscience at the University of Michigan, says—
Psychiatrists prescribe Prozac and the other selective serotonin reuptake inhibitors not only for depression, but also for obsessive-compulsive disorders, panic disorders, various food-related problems (including both anorexia and bulimia), premenstrual dysphoric syndrome (PMS), attention-deficit/hyperactivity disorder (ADHD), borderline personality disorder, drug and alcohol addiction, migraine headaches, social phobia, arthritis, autism, and behavioral and emotional problems in children, among many other conditions.
A February 2011 article in Pharmacoepidemiology and Drug Safety ("Increasing off-label use of antipsychotic medications in the United States, 1995-2008", Vol. 20, Issue 2, pp. 177-184) by Caleb Alexander, M.D., Assistant Professor of Medicine at the University of Chicago, and Randall Stafford, M.D., Ph.D., Associate Professor of Medicine at Stanford Prevention Research Center, et al., says "Although approved initially for schizophrenia, antipsychotic medications also are used for numerous other conditions, including other psychoses, bipolar disorder, delirium, depression, personality disorders, dementia, and autism." In a lecture at the National Educational Alliance—Borderline Personality Disorder (BPD) conference in Atlanta, Georgia on November 4, 2011, psychiatrist Kenneth Silk, M.D., said drugs as diverse as SSRI antidepressants, mood stabilizers, and both typical and atypical antipsychotics have been used as "treatment" for BPD ("Medication: The Positives and the Negatives—Kenneth Silk, MD", YouTube.com at 39:55-41:10). In We've Got Issues—Children and Parents in the Age of Medication (Riverhead Books 2010, p. 171), Judith Warner recalls that "In the late 1970s ... antianxiety meds were being given—rightly or wrongly—as treatment for a wide array of problems, including depression." Why would an "anti-anxiety" drug be used for depression if psychiatric drugs have any specificity rather than a general disabling effect? Reading or hearing such comments from psychiatrists and other mental health professionals and other observers, or paying attention to advertising for psychiatric drugs and seeing some initially advertised as antipsychotic later advertised as useful against depression (e.g., Abilify), or supposed antidepressants advertised as effective in quitting smoking or suppressing obsessive-compulsive disorder or other problems, it eventually becomes difficult to avoid the conclusion that any and every psychiatric drug is used to treat any and every supposed psychiatric problem. All psychiatric drugs are mentally disabling generally and therefore can be used to reduce anything in human thinking or behavior (both good and bad). So why are some called "antianxiety", and others "antipsychotic" or "antidepressant" or "mood stabilizers"? The answer is salesmanship. Claims that any particular type of psychiatric drug is specifically effective against any specific type of psychiatric problem is salesmanship, not science.
According to psychiatrist Daniel J. Carlat, M.D., in his book Unhinged—The Trouble With Psychiatry (Free Press 2010, pp. 83, 84, 86)—
The fact is that psychopharmacology is primarily trial and error, a kind of muddling through different candidate medications until we hit on one that works. ...we rely largely on intangible factors to make these decisions. ... What to do in a case like this, in which the first drug loses its effectiveness? The process of selecting a second agent is guesswork. ... Such is modern psychopharmacology. Guided purely by symptoms, we try different drugs, with no real conception of what we are trying to fix, or of how the drugs are working. [underline added]
In their book Mad Science—Psychiatric Coercion, Diagnosis, and Drugs (Kirk, et al., Transaction Publishers 2013), three social work professors reach a similar conclusion:
Also, together we've amassed over seventy-five years of teaching mental health courses in graduate schools of social work to thousands of students and professionals ... It seems to us, on the other hand, that clinical psychopharmacology—the medically sanctioned use of psychoactive drugs for the treatment of medically legitimated distress and misbehavior (termed mental disorders)—has always been a pseudoscientific enterprise. ... nearly all psychotropic drug classes end up prescribed for all groups of disorders ... there are no demonstrated biological anomalies for any drug to target to "cure" the mental disorders in question. ... no radical innovation based on genetic knowledge is leading the way to find any curative compounds in psychiatry, because there is simply no idea about what specific part of the body, if any, need fixing when people suffer or misbehave. ... Psychoactive drugs, let us note, are prescribed in the absence of demonstrated physical pathology. [pp. 301, 250, 262, 251, 254, 255, italics in original]
According to Jack M. Gorman, M.D., in his book The Essential Guide to Psychiatric Drugs, 4th Edition (St. Martin's/Griffin 2007, p. 6), psychiatrists decide which drug to prescribe on the basis of "clinical lore, experience, and intuition" rather than bona-fide science.
This could be called "The Myth of Psychopharmacology": "...ology" means knowledge. For example, "Nephrology" is knowledge about kidneys, and "psychology" is knowledge of the psyche, or mind. But in the case of "psychopharmacology", the knowledge is absent. "Psychopharmacology", in other words, is a form of quackery.
The haphazard way therapists chose which psychiatric drug to prescribe is also admitted, at least tacitly, in the Handbook of Clinical Psychopharmacology for Therapists, Sixth Edition, (John D. Preston, Psy.D., et al., New Harbinger Publications 2010, pp.179-180), written by a psychologist, a psychiatrist, and a pharmacist. For depression, their advice about choosing a supposedly antidepressant "medication" is mostly about avoiding so-called side-effects. They admit "No antidepressant has been proven consistently superior to another" (p. 170), and "Despite our knowledge of some of the important mechanisms of action of these medications, we still do not really know how they relieve depression" (p. 169). They say "Whichever antidepressant is chosen first, the question of what to try if the first one doesn't work may arise" (p. 179). They suggest "switching classes of antidepressants (i.e., if first treated with an SSRI [selective serotonin reuptake inhibitor], switch to a norepinephrine or dopamine reuptake inhibitor, such as bupropion) versus switching within class (i.e., from one SSRI to another SSRI)" (pp. 179-180, italics theirs).
There is no rational way for a drug prescriber to know one so-called antidepressant will be more effective than another, because there are neither biological nor psychological tests to indicate, for example, that one patient suffers from a type of depression that will be relieved by a tricyclic antidepressant but not a SSRI, another patient a type of depression that will be relieved by a SSRI and not a tricyclic, and another patient a type of depression that will be relieved by a SNRI (serotonin and norepinephrine reuptake inhibitor) but not a tricyclic nor SSRI, and another patient a type of depression that will be relieved only by a MAOI (monoamine oxidase inhibitor). The situation is the same for all psychiatric drugs, such as supposedly antipsychotic and supposedly anti-anxiety drugs. As Dr. Gorman says, it's all "clinical lore, experience, and intuition". That's guesswork, not science.
It is often asserted that taking a psychiatric drug is like taking insulin for diabetes. Although psychiatric drugs are taken continuously, as is insulin, it's an absurd analogy. Diabetes is a disease with a known physical cause. No physical cause has been found for any of today's so-called mental illnesses. The mode of action of insulin is known: It is a hormone that instructs or causes cells to uptake dietary glucose (sugar). In contrast, the modes of action of psychiatry's drugs are unknown—although even advocates of psychiatric drugs as well as critics theorize they prevent normal brain functioning by blocking neuroreceptors in the brain. If this theory is correct it is another contrast between taking insulin and taking a psychiatric drug: Insulin restores a normal biological function, namely, normal glucose (or sugar) metabolism. Psychiatric drugs interfere with a normal biological function, namely, normal neuroreceptor functioning. Insulin is a hormone that is found naturally in the body. Psychiatry's drugs are not normally found in the body. Insulin gives a diabetic's body a capability it would not have in the absence of insulin, namely, the ability to metabolize dietary sugar normally. Psychiatric drugs have an opposite kind of effect: They take away (mental) capabilities the person would have in the absence of the drug. Insulin affects the body rather than the mind. Psychiatric drugs disable the brain and hence the mind, the mind being the essence of the real self.
In the final analysis, "there are no justifiable uses of psychiatric drugs" (Dr. Joanna Moncrieff, The Myth of the Chemical Cure—A Critique of Psychiatric Drug Treatment, Revised Edition, Palgrave Macmillan 2009, p. 15, summarizing the view of Dr. Peter Breggin, which she says "usefully highlights the general character of psychotropic drugs.") I believe adults should have the right to use whatever drugs they want. However, the use of psychiatric drugs by licensed professionals is an example of medical professionals failing to adequately regulate themselves, and the failure of state legislatures, Congress, and regulatory agencies like the USA's Food and Drug Administration (FDA) to protect the public. Peter C. Gøtzsche, a physician specializing in internal medicine, and professor of Clinical Research Design and Analysis at the University of Copenhagen, devotes two chapters to psychiatric drugs in his book Deadly Medicines and Organized Crime — How Big Pharma Has Corrupted Healthcare (Radcliffe 2013). He closes the second of these two chapters with the following words, which he indents and italicizes for emphasis, and with which I will end this essay:
Our citizens would be far better off if we removed all the psychotropic drugs from the market, as doctors are unable to handle them. It is inescapable that their availability creates more harm than good. [p. 233]
Caution: Stopping taking psychiatric drugs abruptly can cause severe, even life-threatening, withdrawal problems. For advice about how to withdraw from psychiatric drugs, see Psychiatric Drug Withdrawal—A Guide for Prescribers, Therapists, Patients, and Their Families (Springer Publishing 2013) by psychiatrist Peter R. Breggin, M.D., or Your Drug May Be Your Problem: How and Why to Stop Taking Psychiatric Medications (Da Capo Press 2007) by Dr. Breggin and clinical social work professor David Cohen.
Books
John Abramson, M.D., Overdosed America—The Broken Promise of American Medicine (Harper Perennial 2008)
Marcia Angell, M.D., The Truth About Drug Companies—How They Deceive Us and What To Do About It (Random House 2005)
Alison Bass, Side Effects—A Prosecutor, A Whistleblower, and a Bestselling Antidepressant on Trial (Algonquin Books of Chapel Hill 2008)
Peter R. Breggin, M.D., Psychiatric Drugs—Hazards to the Brain (Springer Publishing Co., New York, 1983)
Peter R. Breggin, M.D., Toxic Psychiatry—Why Therapy, Empathy and Love Must Replace the Drugs, Electroshock, and Biochemical Theories of the "New Psychiatry" (St. Martin's Press 1991)
Peter R. Breggin, M.D., Talking Back to Prozac (St. Martin's Paperbacks 1994)
Peter R. Breggin, M.D., Antidepressant Fact Book: What Your Doctor Won't Tell You About Prozac, Zoloft, Paxil, Celexa, and Luvox (Perseus 2001) book review
Peter R. Breggin, M.D., and David Cohen, Ph.D., Your Drug May Be Your Problem—How and Why to Stop Taking Psychiatric Medications (Perseus 1999). I read this first 1999 edition. A "Fully Revised and Updated" edition was published in 2007 (by Da Capo/Perseus). book review
Peter R. Breggin, M.D., Brain-Disabling Treatments in Psychiatry, Second Edition (Springer Publishing Co. 2008)
Peter R. Breggin, M.D., Psychiatric Drug Withdrawal—A Guide for Prescribers, Therapists, Patients, and Their Families (Springer Publishing Co. 2013)
Vernon Coleman, M.B.Ch.B., D.Sc.(hon), How to Stop Your Doctor Killing You (European Medical Journal 2003), especially the chapter titled "Why Mental Health Care Isn't Always Worth Having".
Allen Frances, Saving Normal—An Insider's Revolt Against Out-of-Control Psychiatric Diagnosis, DSM-5, Big Pharma, and the Medicalization of Ordinary Life (Harper Collins 2013). I recommend this book despite my disagreement with the author about the validity of the concept of mental disorder and his belief that psychiatry has bona-fide treatment.
Joseph Glenmullen, M.D., Prozac Backlash (Simon & Schuster 2000)
Peter C. Gøtzsche, Deadly Medicines and Organized Crime — How Big Pharma Has Corrupted Healthcare (Radcliffe 2013), especially chapters 17 ("Psychiatry, the drug industry's paradise") and 18 ("Pushing children into suicide with happy pills")
Peter C. Gøtzsche, Deadly Psychiatry and Organized Denial (People'sPress 2015)
Stuart A. Kirk, et al., Mad Science—Psychiatric Coercion, Diagnosis, and Drugs (Transaction Publishers 2013)
Irving Kirsch, Ph.D., The Emperor's New Drugs—Exploding the Antidepressant Myth (Basic Books 2010)
Joanna Moncrieff, M.B.B.S., M.Sc., MRCPsych, M.D., The Myth of the Chemical Cure—A Critique of Psychiatric Drug Treatment, Revised Edition (Palgrave Macmillan 2009)
Joanna Moncrieff, M.B.B.S., M.Sc., MRCPsych, M.D., A Straight Talking Introduction to Psychiatric Drugs (PCCS Books 2009)
Joanna Moncrieff, M.B.B.S., M.Sc., MRCPsych, M.D., The Bitterest Pills—The Troubling Story of Antipsychotic Drugs (Palgrave MacMillan 2013)
Colin A. Ross, M.D., The Great Psychiatry Scam—One Shrink's Personal Journey (Manitou Communications, Inc., Richardson, Texas 2008).
Colin A. Ross, M.D., and Alvin Pam, Ph.D., Pseudoscience in Biological Psychiatry (John Wiley & Sons, Inc. 1995) book review
Elliot Valenstein, Ph.D., Blaming the Brain—The Truth About Drugs and Mental Health (Free Press 1998)
Robert Whitaker, Mad in America (Perseus 2002). In this book, the author documents that fact that people considered insane or mentally ill were more likely to recover and live good lives before the invention of modern biological psychiatry (psychiatric drugs, electroshock, and psychosurgery).
Robert Whitaker, Anatomy of an Epidemic—Magic Bullets, Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America (Crown Publishers 2010). In this sequel to Mad in America, Robert Whitaker reviews the evidence of harm caused by each class of psychiatric drugs and documents the increase in mental disability and illness caused by their use.
Ginger Ross Breggin, "On Being Human", empathictherapy.org
Dr. Peter Breggin, "New Research: Antidepressants Can Cause Long-Term Depression", Huffington Post (huffingtonpost.com), 11/16/2011
Monica Cassani, "How antidepressants (and benzos) ruined my life: Luke Montagu", July 18, 2015 — Beyond Meds: Alternatives to Psychiatry, http://beyondmeds.com
"High Anxiety", January 1993 Consumer Reports magazine
Siphiwe Sibeko, "Psychiatric Drugs Kill 500,000 Western adults annually, few positive benefits — leading scientist", rt.com, May 13, 2015; original article: "Does long term use of psychiatric drugs cause more harm than good?", British Medical Journal, 12 May 2015.
Julia Llewellyn Smith, "Lives 'left in ruin' by rising tide of depression drugs", The Telegraph (UK), 27 April 2014
"Psychiatric Drugs Are More Dangerous Than You Ever Imagined", YouTube.com and breggin.com. This is an excellent 9-minute video by Dr. Peter Breggin that should be seen by anyone and everyone taking, prescribing, or advocating the use of psychiatric drugs.
"Psychiatry causes harm, and it's widely denied...", YouTube.com. In this less than 2 minute video, Joanna Moncrieff, a psychiatrist and senior lecturer in Mental Health Sciences at the University College, London, summarizes the evidence showing psychiatric drugs harm people and that most of her fellow psychiatrists don't care.
A Psychiatrist's Perspective on Antidepressants (Kelly Brogan, M.D.), YouTube.com.
Dr. Peter Breggin testifying before U.S. House of Representatives Committee on Veterans' Affairs about newer (SSRI) antidepressants causing suicide; also available on YouTube.com.
"Generation Rx", by Kevin P. Miller, available on DVD from amazon.com and usually also on eBay.com, not to be confused with the A&E film by the same title. See amazon.com.
"The Drugging of Our Children", A Gary Null Production, garynull.com, available from amazon.com.
"NUMB: A Documentary, The Depressing Truth About Antidepressants". Watch this documentary before starting or stopping an SSRI antidepressant such as Paxil. This documentary illustrates the fact that psychiatric drugs such as SSRIs are often much easier to start than to stop and that even tapering off them slowly may be unsuccessful. The film ends with the film maker switching from Paxil to Prozac but being unable to stop taking SSRI "antidepressants" without intolerable withdrawal symptoms. See numbdocumentary.com.
"Psychiatric Drugs and Mass Shootings", YouTube.com. This video provides evidence psychiatric drugs cause violent behavior, contrary to the common view about mentally ill people needing to be "stabilized on meds" to prevent violence. I recommend this Citizens Commission on Human Rights (CCHR) video without endorsing CCHR itself nor the founder of CCHR, the Church of Scientology: See comment in The Future of Anti-Psychiatry Activism.
Permission to reproduce is granted
provided the reproduction is accurate
and proper credit is given
The author is a volunteer (pro bono) attorney for the Law Project for Psychiatric Rights (psychrights.org) and may be reached at wayneramsay (at) mail (dot) com
[ Contents | Next Essay: "Psychiatry's Electroconvulsive Shock Treatment" ]